The spine includes cervical, thoracic, and lumbosacral vertebrae, and is composed of 33-34 vertebrae that are arranged up and down and connected into a single chain.In order to evenly distribute the load on the spine during daily physical activities, the spine has a physiological (normal) curvature when the body is in an upright position.There are two curves that bulge forward (lordosis) in the cervical and lumbar region, and two curves that bulge backward (kyphosis) in the thoracic and sacral regions.Between the vertebrae are intervertebral discs - cartilage that has a shock-absorbing function and consists of the nucleus pulposus and the surrounding annulus fibrosus.
Spinal osteochondrosis is a chronic disease characterized by degenerative dystrophic changes in the intervertebral discs, subsequently involving adjacent vertebrae and surrounding tissues in the process.
Currently, doctors more commonly use the broader term "back pain" to refer to back and neck pain, sometimes replacing the concept of "osteochondrosis."Back pain includes neck pain (cervical pain), neck and head pain (cervical pain), neck and shoulder pain (cervical pain), chest pain (chest pain), low back pain (lumbar pain), and low back pain that radiates to the legs (lumbar pain).
Causes of spinal osteochondrosis
To date, there are no firm data on the causes of degenerative changes in the spine.There are many theories taking into account various factors: involution (involution - reverse development, backward movement), mechanical, immune, hormonal, metabolic disorders (metabolism), vascular, infectious, functional and genetic.The most common is the degeneration theory, according to which local premature aging of cartilage and bone occurs due to previous mechanical or inflammatory damage.According to this theory, the occurrence of spinal degenerative changes is predetermined by genes, and the occurrence of diseases with corresponding clinical manifestations is due to the influence of various endogenous and exogenous factors.
The likelihood of osteochondrosis increases with age due to excess weight, a sedentary lifestyle and poor physical fitness on the one hand, and heavy manual labor and vibration exposure on the other.
The load on the spine increases proportionally with body weight, so that overweight people experience overloading even with moderate activity; this situation is aggravated by a tendency to lack physical activity due to poor tolerance for physical activity.
Psycho-emotional stress combined with a sedentary lifestyle can lead to changes in individual muscle group tension, muscle tone, and movement patterns (posture, gait).Scoliosis – The development of scoliosis, pathological kyphosis, and lordosis (worsening of physiological curves) can also lead to disc deformation.
Disease classification
By localization:
- Cervical osteochondrosis;
- Thoracic osteochondrosis;
- Osteochondrosis of the lumbar and sacral spine.
Depending on the stage of the disease:
- exacerbations (maximum number of clinical manifestations);
- Remission (no clinical manifestations).
Depending on which structures are affected by the pathology, the affected spinal structures can be divided into:
- Reflex syndromes - reflex tension in innervated muscles, or myotonic disorders (muscle spasms), vascular, vegetative, dystrophic - occur when pain receptors are stimulated.
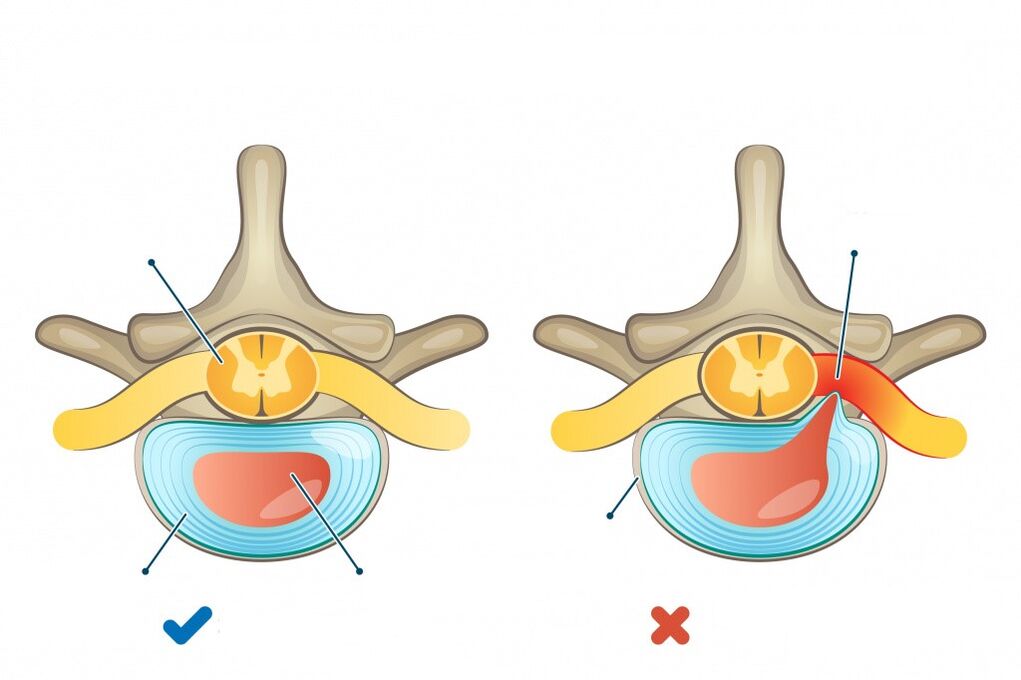
- Compression syndrome usually occurs in the context of disc herniation (herniation, protrusion of the disc outside the spine without compromising the integrity of the annulus fibrosus) or disc herniation (radiculopathy, neuropathy, myelopathy, radicular ischemic syndrome are distinguished accordingly) due to compression of nerve roots, spinal cord or blood vessels.
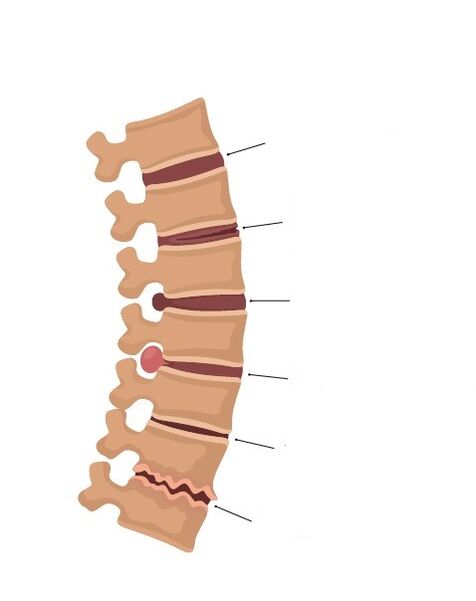
Depending on the development stage of the process, there are:
- Stages of intradiscal pathological processes (chondrosis).During this period, intradiscal movement of the nucleus pulposus occurs.The nucleus pulposus penetrates into its outer fibers through the fissures in the annulus fibrosus.As a result, the nerve endings become irritated and produce pain.
- A stage in which the affected disc becomes unstable or loses its ability to hold in place when the overlying vertebrae become displaced relative to the underlying vertebrae.During this period, instability syndromes, reflexes, and even compression syndromes can develop.
- The stage in which a disc herniation develops due to a violation of the integrity of the annulus fibrosus, which compresses adjacent neurovascular structures, including spinal nerve roots.
- The stage of disc fibrosis and the formation of osteochondral growth at the vertebral body margins lead to vertebral immobility and a compensatory increase in the supporting area of the defective disc.In some cases, these bony growths (such as a herniated disc) can compress adjacent neurovascular structures.
Symptoms of osteochondrosis
Symptoms of osteochondrosis depend on where the spine is damaged and the extent of the changes, and the function of internal organs may be impaired.
Cervical osteochondrosis is characterized by neck pain that worsens with movement, radiates to the arms, and is accompanied by numbness in the fingers.
Symptoms may include headache in the occipital area, dizziness, ringing in the ears, dark eyes, or flashing spots in front of the eyes.
When the thoracic spine is affected, patients may experience pain in the heart area and interscapular area, which lasts for a long time, soreness or pressure, and is often sharp, stabbing, and sharp.
They may occur or worsen with deep breathing, bending and turning the body, raising arms, sneezing, or coughing.The skin on the chest, abdomen, and back may feel numb.
Patients with lumbosacral osteochondrosis will experience stiffness of movement and lower back pain. The pain can radiate to one or both legs, and is aggravated when bending, turning, walking, or lifting heavy objects.
Possible vegetative disease: coldness in the legs, comfortable temperature in other parts of the body, pale skin on the legs.Feelings of numbness and paresthesia (pins and needles) on the skin of the legs and buttocks.
Diagnosis of disease
Instrumental diagnosis involves radiographic examination of the spine to rule out trauma, congenital structural anomalies, and identify bone growth.The study also performed functional tests - taking pictures during flexion and extension of the cervical and lumbar regions to rule out pathological displacement of the vertebrae relative to each other.






















